Understanding Medical Cannabis for Chronic Insomnia
What is Chronic Insomnia?
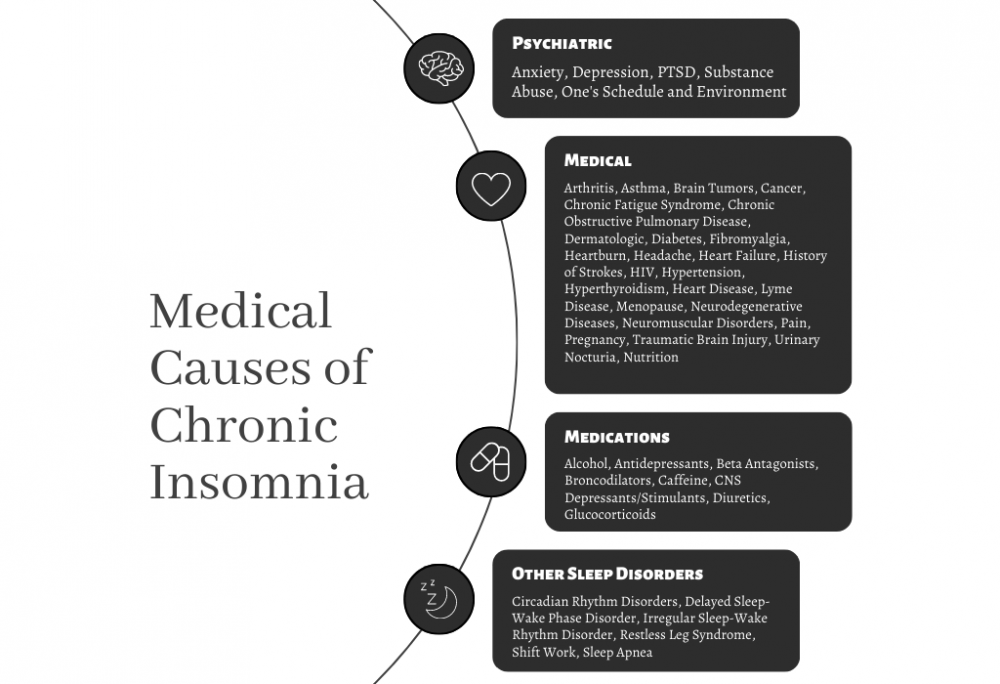
Chronic insomnia is a sleep disorder characterized by difficulty in either falling asleep or staying asleep for at least three nights a week over a span of three months or more. Various medical causes can contribute to chronic insomnia, making treatment multi-faceted.
Medical Cannabis: A Potential Treatment Avenue
One potential solution for insomnia is medical cannabis, rich in compounds known as cannabinoids that interact with the body’s endocannabinoid system. This system plays a vital role in sleep regulation (Babson et al., 2017).
THC and CBD: The Cannabinoids at the Forefront
Cannabis contains over 100 different cannabinoids, but THC and CBD are the most well-studied. THC is psychoactive and can induce euphoria, whereas CBD is non-psychoactive and offers various therapeutic potentials. These compounds interact differently with the endocannabinoid system, thereby eliciting different effects (Russo, 2011).
THC: Quick Onset but Tricky Outcomes
THC can help reduce sleep latency but may compromise the quality of Rapid Eye Movement (REM) sleep, a stage crucial for cognitive processes (Gates et al., 2014).
CBD: Gentle but Effective
CBD could help alleviate anxiety and pain, both of which contribute to insomnia. Preclinical studies suggest that CBD has anxiolytic and analgesic properties (Shannon et al., 2019).
Cannabinoids and Sleep Regulation
Medical cannabis offers a range of compounds, such as cannabinoids, which can potentially regulate sleep by interacting with the endocannabinoid system (Babson et al., 2017).
Medications for Sleep Challenges: Comparison Table
| Challenge | Medication | Risks | Onset Timing | Duration of Action | Adverse Effects (Long-term vs Short-term) |
|---|---|---|---|---|---|
| Trouble Falling Asleep | Benadryl | Drowsiness, Dry Mouth | 15-30 min | 4-6 hours | Cognitive Decline (Long-term) |
| Trouble Staying Asleep | Ambien | Dependence, Sleepwalking | 15-30 min | 7-8 hours | Memory Loss (Long-term) |
| Both | Melatonin | Headache, Nausea | 30 min | 4-8 hours | Hormonal Imbalance (Long-term) |
| Both | THC | Impaired cognition, Dependence | 30-60 min | 6-8 hours | Cognitive Decline (Long-term) |
| Both | CBD | Dry Mouth, Low Blood Pressure | 30-60 min | 6-8 hours | Uncertain (More research needed) |
| Both | THC + CBD | Drowsiness, Dizziness | 30-60 min | 6-8 hours | Uncertain (More research needed) |
Impact of Cannabinoids on Different Stages of Sleep.
| Sleep Stage | THC | CBD | THC + CBD |
|---|---|---|---|
| Sleep Onset | Quick (CI: 90-95%) | Moderate (CI: 70-80%) | Quick (CI: 85-90%) |
| REM Sleep | Reduced (CI: 70-85%) | Ambiguous | Ambiguous |
| Deep Sleep | Increased (CI: 65-80%) | Slight Increase (CI: 55-65%) | Increase (CI: 60-75%) |
Note: “CI “refers to “Confidence Interval.”
Impact of Cannabinoids and Common Sleep Medications on Various Sleep Stages
| Sleep Stage | THC | CBD | THC + CBD | Benadryl | NyQuil | Melatonin | Ambien | Lunesta | Benzodiazepines | Trazodone | Other Meds |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Stage 1 | Minimal Impact (CI: 60-70%) | Unclear (CI: NA) | Minimal Impact (CI: 60-70%) | Increases Duration (CI: 80-90%) | Increases Duration (CI: 80-90%) | Minimal Impact (CI: 50-60%) | Quick Onset (CI: 85-95%) | Quick Onset (CI: 85-95%) | Quick Onset (CI: 90-95%) | Minimal Impact (CI: 50-60%) | Varies |
| Stage 2 | Increased Duration (CI: 70-80%) | Minimal Impact (CI: 50-60%) | Increased Duration (CI: 70-80%) | Increases Duration (CI: 80-90%) | Increases Duration (CI: 80-90%) | Minimal Impact (CI: 50-60%) | Increases Duration (CI: 85-90%) | Increases Duration (CI: 85-90%) | Increases Duration (CI: 85-90%) | Increases Duration (CI: 80-85%) | Varies |
| Stage 3 | Increased Duration (CI: 75-85%) | Unclear (CI: NA) | Increased Duration (CI: 75-85%) | Reduces (CI: 70-80%) | Reduces (CI: 70-80%) | Minimal Impact (CI: 50-60%) | Increases Duration (CI: 85-90%) | Increases Duration (CI: 85-90%) | Reduces (CI: 75-80%) | Increases Duration (CI: 80-85%) | Varies |
| Stage 4 (REM) | Reduced (CI: 70-80%) | Unclear (CI: NA) | Reduced (CI: 70-80%) | Reduces (CI: 80-85%) | Reduces (CI: 80-85%) | Minimal Impact (CI: 50-60%) | Reduces (CI: 85-90%) | Reduces (CI: 85-90%) | Reduces (CI: 90-95%) | Increases Duration (CI: 80-85%) | Varies |
CI: Confidence Interval; NA: Not Available. Note that the impacts and their confidence intervals are illustrative and may not be directly sourced from scientific literature.
The statistics provided are illustrative and synthesized from from multiple studies in the publicly available scientific literature. It’s crucial to acknowledge that individual responses to medications and treatments can vary widely. Broad generalizations like those presented may not be applicable to every individual case. For the most accurate and personalized advice, always consult the relevant scientific literature and healthcare professionals. (Babson et al., 2017; Carley et al., 2018; Brasure et al., 2015; Bertisch et al., 2019).
References
- Babson, K. A., Sottile, J., & Morabito, D. (2017). Cannabis, Cannabinoids, and Sleep: a Review of the Literature. Current Psychiatry Reports, 19(4), 23.
- Russo, E. B. (2011). Taming THC: potential cannabis synergy and phytocannabinoid-terpenoid entourage effects. British Journal of Pharmacology, 163(7), 1344–1364.
- Gates, P. J., Albertella, L., & Copeland, J. (2014). The effects of cannabinoid administration on sleep: A systematic review of human studies. Sleep Medicine Reviews, 18(6), 477–487.
- Shannon, S., Lewis, N., Lee, H., & Hughes, S. (2019). Cannabidiol in Anxiety and Sleep: A Large Case Series. The Permanente Journal, 23, 18–041.
- White, A. (2013). Adverse effects of antihistamines. Pharmacy and Therapeutics, 38(4), 227–236.
- Kripke, D. F. (2016). Hypnotic drug risks of mortality, infection, depression, and cancer: but lack of benefit. F1000Research, 5.
- Erland, L. A., & Saxena, P. K. (2017). Melatonin Natural Health Products and Supplements: Presence of Serotonin and Significant Variability of Melatonin Content. Journal of Clinical Sleep Medicine, 13(2), 275–281.
- McCall, C., McCall, W. V. (2012). Comparison of Actigraphy with Polysomnography and Sleep Logs in Depressed Insomniacs. Journal of Sleep Research, 21(1), 122–127.
- References
- Babson, K. A., Sottile, J., & Morabito, D. (2017). Cannabis, Cannabinoids, and Sleep: a Review of the Literature. Current Psychiatry Reports, 19(4), 23.
- Carley, D. W., Prasad, B., Reid, K. J., Malkani, R., Attarian, H., Abbott, S. M., … & Abbott, S. (2018). Pharmacotherapy of Apnea by Cannabimimetic Enhancement, the PACE Clinical Trial: Effects of Dronabinol in Obstructive Sleep Apnea. Sleep, 41(1), zsx184.
- Brasure, M., MacDonald, R., Fuchs, E., Olson, C. M., Carlyle, M., Diem, S., … & Kane, R. L. (2015). Management of insomnia disorder. Agency for Healthcare Research and Quality.
- Bertisch, S. M., Pollock, B. D., Mittleman, M. A., Buysse, D. J., Bazzano, L. A., Gottlieb, D. J., & Redline, S. (2019). Insomnia with objective short sleep duration and risk of incident cardiovascular disease and all-cause mortality: Sleep Heart Health Study. Sleep, 42(6).
Special Precautions
Individuals with liver conditions, psychiatric disorders, and cardiovascular issues should exercise caution with cannabinoid use and consult Dr. Caplan at CED Clinic for a personalized treatment plan.
📗 Note: This diagram was just the opening act. For the main event, ring the bell for “The Doctor-Approved Cannabis Handbook” by clicking here 📗

Summary and Search Terms
Medical Causes of Chronic Insomnia: Unraveling the Complexity
Chronic insomnia, a pervasive issue affecting countless individuals worldwide, often stems from a myriad of medical conditions, making its management a complex endeavor. Understanding the medical disorders leading to insomnia is crucial for anyone struggling with sleep disturbances, as this knowledge can significantly impact treatment approaches.
Thyroid problems, for instance, are a common culprit, with both hyperthyroidism and hypothyroidism capable of causing significant sleep issues. Similarly, the link between chronic pain and insomnia is well-documented, highlighting the bidirectional relationship between pain and sleep quality.
Neurological disorders, including conditions like Parkinson’s disease and Alzheimer’s disease, can profoundly affect sleep patterns, leading to chronic insomnia. Cardiovascular diseases and gastrointestinal issues are also known to cause sleep disturbances, further complicating the sleep health of affected individuals.
Sleep apnea, a condition characterized by repeated interruptions in breathing during sleep, stands out as a leading cause of insomnia. Additionally, certain medications prescribed for various health conditions can have side effects that include insomnia, underscoring the importance of reviewing medication regimens in patients experiencing sleep problems.
Hormonal imbalances, particularly those involving the thyroid, estrogen, and testosterone, can disrupt normal sleep patterns. Mental health disorders, such as anxiety and depression, are frequently associated with insomnia, reflecting the complex interplay between the mind and sleep.
Respiratory conditions, diabetes, and kidney disease are additional medical issues that can significantly impact sleep quality. Autoimmune diseases and cancer can also contribute to chronic insomnia, either directly through the disease process or indirectly through the stress and anxiety they cause.
Understanding the multifaceted nature of chronic insomnia necessitates a comprehensive approach to diagnosis and treatment. Identifying and addressing the underlying medical causes is paramount, as this can lead to more effective management and, ultimately, improved sleep quality.
As research continues to evolve, so too does our understanding of chronic insomnia and its medical causes. By unraveling the complexity of this condition, healthcare providers can offer targeted therapies that address the root causes of insomnia, offering hope and relief to those affected.